In India, a doubly neglected tropical disease
The parasitic disease kala-azar, or black fever, may lead to a secondary illness, which can spark new infections.
- 20 October 2023
- 8 min read
- by Undark

Up until a few years ago, Sanjeet Pahan didn’t consider visiting a doctor for his skin. But by 2020, small pink lesions had started appearing on his feet. Now, the spots, which resemble red grapes in some places and small berries in others, have spread, reaching all the way up to his face.
Doctors told him the condition wasn’t anything to be afraid of, said Pahan, who lives in a village in West Bengal, India. Like many of his neighbors, Pahan lives in a mud house with a roof made of bamboo and tin, with no safe drinking water or sanitation. Lightbulbs hang loose from the ceiling, and the village buzzes with mosquitoes and flies. “Doctors tell me that I caught kala-azar when I was a kid,” he added.
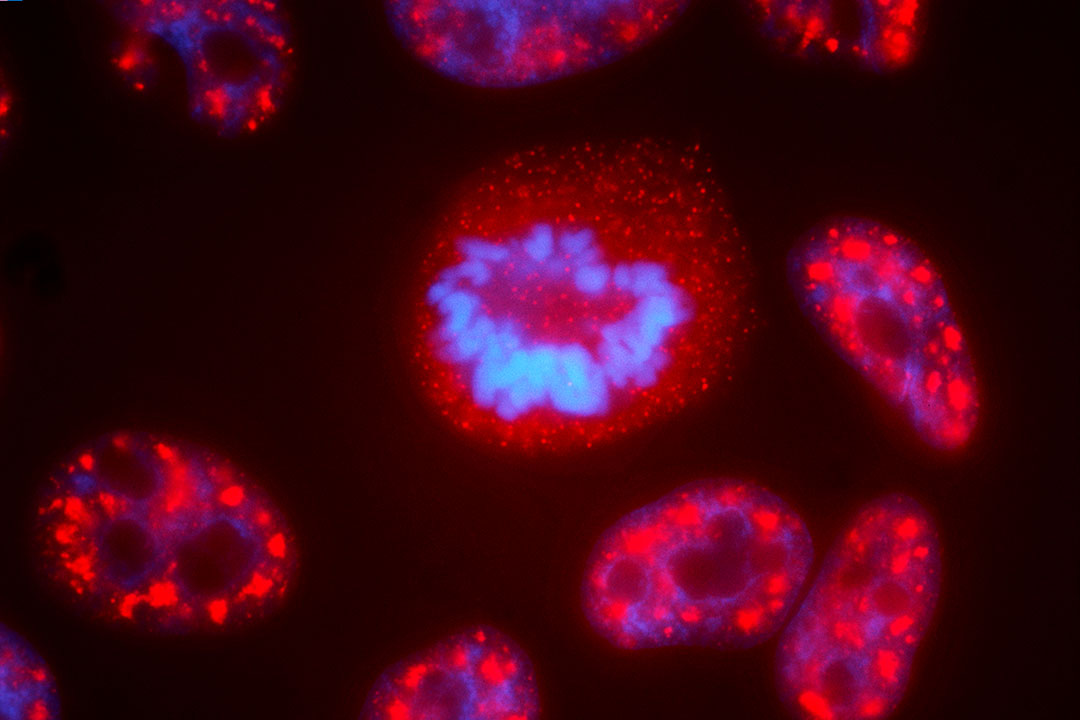
Kala-azar, also called visceral leishmaniasis or black fever, is one of the most neglected tropical diseases in the world, with more than 1 billion people at risk. It is endemic to more than 83 countries, and people from just seven countries — Brazil, Ethiopia, India, Kenya, Somalia, South Sudan, and Sudan — make up 90 percent of the cases. Although reports of kala-azar date back to the 19th century, scientists still don’t understand much about how and why it manifests. What is known is that kala-azar is caused by Leishmania parasites, which spread through sandfly bites. The infection can cause fever and enlargement of the liver and spleen, among other symptoms. If left untreated, kala-azar kills more than 95 percent of its victims — it’s the second deadliest parasitic disease after malaria.
Although cases of kala-azar have decreased, thanks in part to successful treatment programs, it can be followed by a complication called post-kala-azar dermal leishmaniasis, or PKDL, which continues to be a threat. The disease — which causes skin issues such as scaly patches and nodular lesions — “is not a life-threatening condition” by itself, said Tarik Jašarević, a spokesperson for the World Health Organization, by email. “However, it causes stigma and discrimination.”

Credit: Monika Mondal for Undark
And although PKDL itself is not fatal, people who are infected with the disease can spread kala-azar to new hosts.
This complication is what Pahan has, according Aditya Adhikary, who was a junior resident doctor at the Institute of Post Graduate Medical Education & Research in Kolkata when he visited Pahan. “He is an extreme case of PKDL,” Adhikary said. If PKDL cases continue to rise, some research suggests, kala-azar may increase as well.
Aside from the connection to kala-azar, experts aren’t sure what causes PKDL. Medicines exist, but they are expensive, difficult to access, and don’t always work. As the climate is getting warmer, the sandflies that spread kala-azar are expanding their territory, too, potentially infecting more people.
Mitali Chatterjee, a pharmacology professor at the Institute of Postgraduate Medical Education & Research, said that kala-azar is considered a neglected tropical disease because it affects mostly poor communities in tropical areas. And because PKDL appears only in “the poorest of the poor,” Chatterjee added, this secondary infection is “a neglected component of a neglected tropical disease.”
Over the past decade or so, kala-azar infections have decreased in India, from 9,241 cases and 11 deaths in 2014 to 818 cases and three deaths in 2022. Over that same time period, PKDL cases rose from 421 to 616. The latter disease peaked in 2017, with 1,982 cases, and some experts who spoke with Undark think that there may be far more cases today than are reported, as government funding for tracking virtually disappeared during the Covid-19 pandemic. “The active case search operations have decreased,” said Uttam Sarkar, a local health worker. When it comes to funding, “it saddens me to say it out loud, but no, we don’t have any,” he added.
According to Chatterjee, the lower numbers of kala-azar are due in part to an elimination program that identifies patients and treats them with an antiprotozoal drug called liposomal amphotericin B.
People who go on to contract PKDL can also take liposomal amphotericin B, but it’s an injection typically given under medical supervision. The only oral medication for PKDL is miltefosine, which is on the WHO’s list of essential medications. All of the drugs on the list are selected based on how common a disease is and how relevant those drugs are to public health, as well as how safe and effective they are. But miltefosine doesn’t always cure the condition. One study, for instance, suggests that the drug may only cure about 85 percent of cases.
It's also difficult to get the drug. Miltefosine is not available in local or private pharmacies in India and is even difficult for health care workers to access. There is no medicine, said Sarkar. He added that people are frustrated with the lack of treatment, and have sometimes taken their frustrations out on health care workers. “So, we are sitting in here helpless, unable to contact them out of fear.”
The WHO invested in miltefosine as a treatment for leishmaniasis through a public-private partnership that was intended to make the medicine widely and affordably available to countries, and free for patients. But now, the government of India is the sole buyer of the drug in that country, a change meant to save patients the need to purchase the drug for the equivalent of $150 to $200 per treatment at private pharmacies. Yet clinicians report ongoing difficulties with availability, affordability, and even securing reliable access to the drug. (Jašarević, the WHO spokesperson, did not respond to questions regarding the miltefosine manufacturing contracts.)

Credit: Monika Mondal for Undark
Have you read?
Even when people can access the medicine, it is difficult to convince them to take it, according to Chatterjee. Miltefosine must be taken for 84 days. It also has a lot of side effects, Chatterjee said, including “nausea, vomiting, and diarrhea” as well as vision loss. Also in many cases, the skin lesions remain for six to 12 months, even after treatment.
According to unpublished research from Chatterjee, about 70 percent of patients say that they were not happy or satisfied with the results of the medicine. “They're not motivated to take the treatment,” said Chatterjee. “This is something which is the major limitation.”
Still, Pahan said that if and when he can access miltefosine, he will take it: “They ask me to wait. So, I am waiting for the medicines to arrive.”
Both kala-azar and PKDL can also be curbed through prevention. Since the 1990s, the central government of India has attempted to eliminate kala-azar, launching projects like the National Vector Borne Disease Control Program. For this program, the government is supposed to regularly survey remote tribal villages, like the one where Pahan lives, identifying people with kala-azar and PKDL, and then spraying their houses and neighborhoods with insecticides.
India’s health department has also recommended providing houses made of concrete for communities with high incidences of kala-azar, to limit the hospitable environment for the flies to grow and breed.
Flies infected with the parasite that causes kala-azar live in the cracks of mud houses, which provide the insects damp and dark places to thrive and reproduce, then spread kala-azar by biting people.

Credit: Monic´ka Mondal for Undark
In 2003, the government began providing cash assistance to states with endemic kala-azar, and incentivizes kala-azar patients to complete treatment with up to 1,700 rupees (equivalent to about $20), according to India’s 2014 National Roadmap for Kala-azar Elimination. Sarkar, the health care worker, said some PKDL patients are now receiving 4,000 rupees (about $50), up from 2,000. This money was meant to cover wage losses. But according to local health workers, the money is not enough to compensate for all the loss for tribal people like Pahan, who are among the poorest in India. Payments, they added, can also be painfully slow.
Some people aren’t even aware the program exists. “They have not told me anything about it,” Pahan told Undark. All he knows, he said, is that someone will eventually give him medicine for his ailment, and it will be given for free.
The relevant government agencies, both of which are with the Government of India’s Ministry of Health and Family Welfare, did not respond to a request for comment: The National Center for Vector Borne Diseases Control and the Central Medical Services Society.
An increase of travel to and from regions like the one where Pahan lives may be pushing the disease to new places across the country. Pahan, for instance, was a migrant worker in southern India when he first contacted a doctor; now, he lives in the east in the same house with two women and two men. Children and older relatives from nearby villages visit his family regularly.
“The sad reality is the patients might not survive because people here are severely malnourished.”
The disease can also be isolating. Young people may be more vulnerable to PKDL compared to other groups, research suggests. During a visit with Pahan, an older relative announced: “But who will marry him with these spots? First, they should go away, and then we can think of marriage.”
“There is a lot of stigma,” Chatterjee told Undark. Through no fault of their own, patients like Pahan, she added, “become marginalized.”
People in communities like Pahan’s are particularly vulnerable. “There are communities where people have roads, electricity, and water, but then you cross their area and enter into tribal communities, there are kala-azar patients,” said Sarkar. “The sad reality is the patients might not survive because people here are severely malnourished.”
Helping them will be difficult, he said. As for eradicating PKDL by the decade’s end, he added: “It's impossible to eliminate the disease.”
Written by
Monika Mondal is an independent journalist based in New Delhi, India. Her work focuses on the environment, agriculture, and sustainability.
Website
This article was originally published by
This article was originally published on Undark on 18 October. Read the original article.