Togo has a cancer problem, but the government says vaccines will help
In 2022, nearly two thirds of the Togolese people diagnosed with cancer died. Vaccination can help change those figures, say Ministry of Health officials.
- 1 September 2025
- 5 min read
- by Nephthali Messanh Ledy
On a Friday morning in August, several women arrive at the Kovié Medical and Social Centre (CMS), about 25 kilometres northwest of the capital Lomé, in the commune of Zio 2, to have their infants vaccinated.
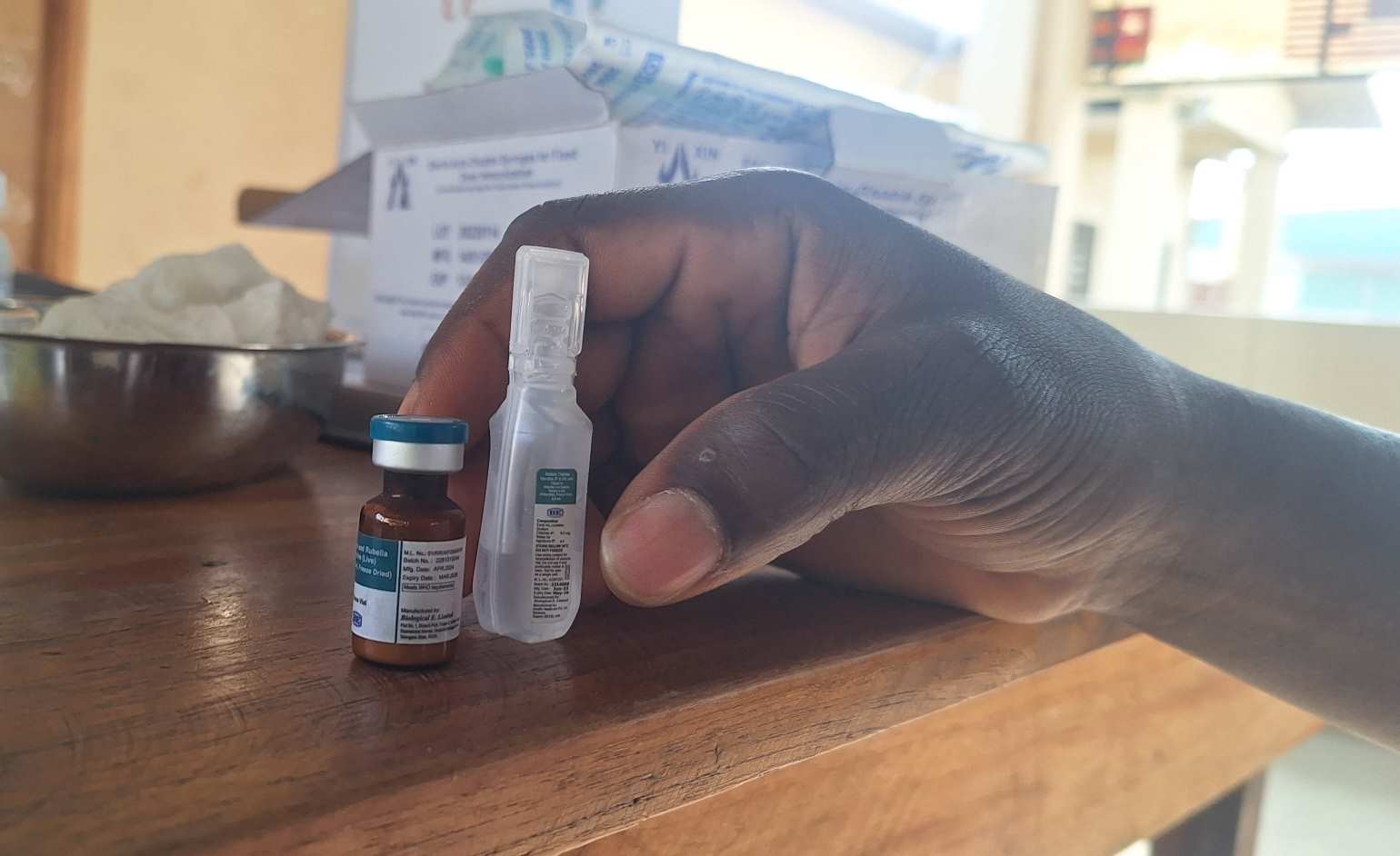
“We were given an appointment for vaccination this morning, that’s why we’re here,” explains one of the women to a health worker on arrival. On the schedule for the day: vaccines from the Expanded Programme on Immunization (EPI), including the pentavalent vaccine, which protects children against five dangerous diseases, among them hepatitis B.
Hepatitis B is a virus that can cause a chronic infection, a nurse explains. If left untreated, it can progress to cirrhosis and, eventually, liver cancer.
Warding off cancer early
The hepatitis B vaccine is not the only jab on the Togolese immunisation schedule that has the power to ward off cancer. The human papillomavirus (HPV) vaccine, which is capable of fending off more than 90% of cervical cancers, was introduced to the country’s immunisation programme with Gavi support in 2023. The babies at the health centre today are years too young – HPV vaccination is recommended for girls aged 9 to 14 – but it’s never too early to inform their parents.
So, as the health team takes a moment to explain the benefits of vaccination, they also talk about the HPV jab.
“This vaccination is for your children, specifically girls aged 9 to 14,” a vaccinator tells them. “We rarely see candidates for this vaccine here at the health centre, but we administer many in schools and during workshops: mostly in schools, since that’s where our target group is.”
“At school, we first raise awareness among the pupils, who then pass the information on to their parents. On the day of vaccination, the girls come with parental consent, and we proceed with the injection,” he explains.
Dr Michel Oni Djanikpo, head of screening at the Togolese Cancer League, a federation of associations active in the fight against cervical cancer, explains that periodic campaigns help to turbocharge the reach of the still relatively unfamiliar vaccine. “These are also opportunities to strengthen awareness, reach communities directly and ensure that more people are protected,” he says.
Credit: Nephthali Ledy
Tackling the “painful reality” of cancer in Togo
According to estimates from the International Agency for Research on Cancer (IARC) for 2022, Togo recorded 5,491 new cancer cases that year. There were also 3,605 deaths - an alarmingly high mortality rate that hints at systemically late diagnoses. “These figures reflect a painful reality and highlight the urgent need for concerted, structured and sustainable action,” said Dr Kokou Wotobé, Secretary General of the Ministry of Health and Public Hygiene of Togo, at a July press conference in Lomé.
To address this challenge, the government has developed and implemented a National Cancer Control Plan (PNLC) for the period 2022–2025. This strategic framework aims to promote screening for breast, cervical, prostate and colon cancers; encourage vaccination against oncogenic viruses; improve diagnosis, treatment and patient care; and strengthen research and surveillance.
But the upstream fight against cancer, which prominently includes vaccination, is not without obstacles. “We sometimes face cases of misinformation about vaccine side-effects,” explains Francis Komlavi Donyoh, senior public health technician in charge of vaccination at the Kovié CMS, noting that schools are particularly sensitive environments. In his view, the role of teachers in relaying accurate information to pupils and parents is key to expanding coverage of HPV vaccination among young girls.
At the Togolese Cancer League, teams stress that prevention structures must cope with limited resources – whether equipment, training or staff – which makes it difficult to scale up interventions nationwide.
Have you read?
Limited access to screening and treatment
Beyond vaccination, access to cancer screening and treatment remains a major challenge. Many patients, living in financially precarious conditions, struggle to afford medical follow-up. Periodic free screening campaigns are organised, including in February for World Cancer Day, in October for Pink October, and in November for Blue November. Some health facilities also reduce their fees to reach more people. But these initiatives remain limited in scope and unevenly distributed across regions.
“We still have a long way to go: we must do everything possible so that everyone, wherever they live, can be screened, treated and supported by qualified health professionals,” concludes Dr Djagnikpo.