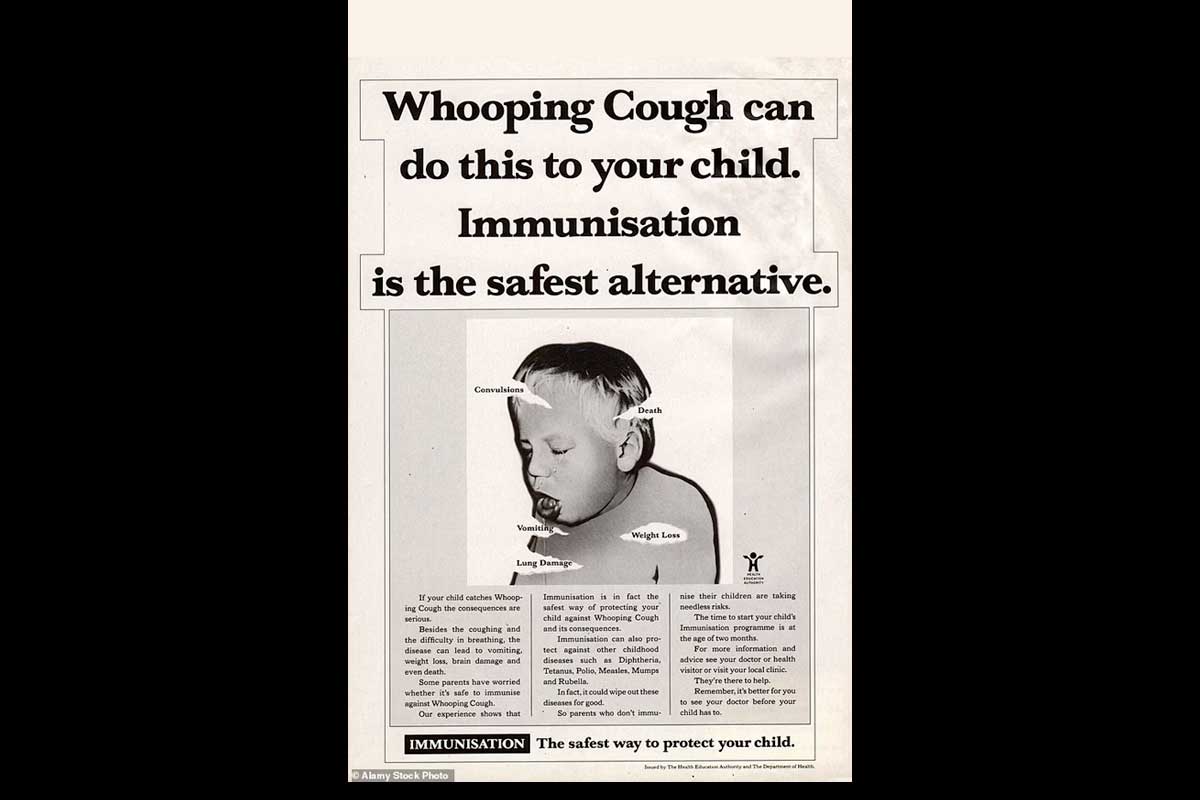
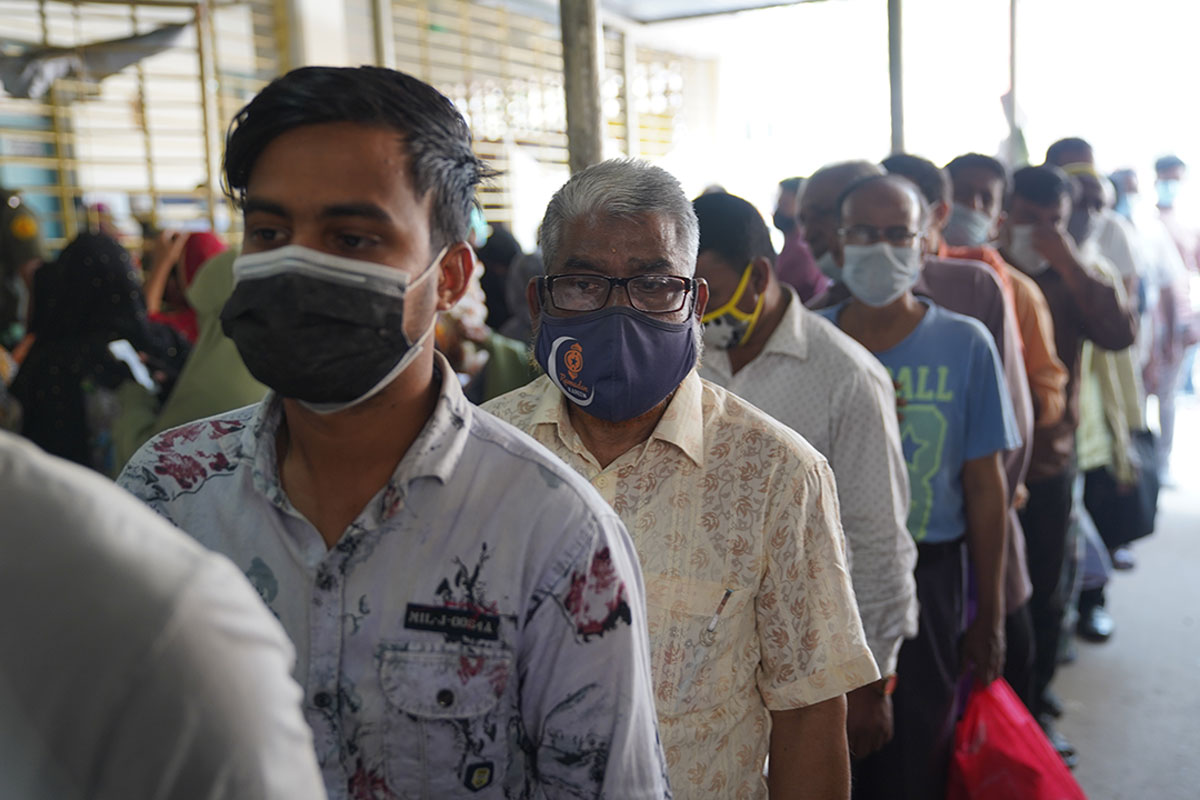
Twelve million vaccinations in three days: how Bangladesh used a pandemic lull to shore up its defences. Credit: Gavi/2022/Saydul Fateheen Murad
Bangladesh’s COVID-19 fatality rates are at an all-time low – but that hasn't stopped the country’s vaccination programme from flooring the gas pedal.
- 1 April 2022
- 6 min read
- by Maya Prabhu
Saturday, 26 February promised to be a pleasant spring day in the greater Dhaka area: no chance of rain, relatively low chance of COVID-19.
In fact, the COVID case count had been in steep decline across Bangladesh for about a month. In the week to 28 February, there would be fewer than 10,000 new cases recorded, and 68 deaths – a 53% reduction against the preceding week’s fatalities. Even in densely-populated Dhaka, typically the nation’s epidemiological epicentre, ICU wards had plenty of beds to spare.
“Mass vaccination solves two key barriers – ease of geographical access and favourable timing, but also positive peer influence. Peers are likely to get vaccinated once they see their colleagues get vaccinated.”
But if the population was experiencing a sense of increasing safety, that didn’t seem to equal complacency. A massive campaign targeting 10 million new vaccinations countrywide in 24 hours was kicking off, and that Saturday morning at health centres across the capital zone, queues spilled out of buildings, snaked out of campus gates and trailed down sun-washed streets.
At the TB Hospital in busy Shyamoli, health workers in pickle green worked double time, relay-style. Practised hands ripped open syringe wrappers and measured up doses of vaccine. Other hands took over, flicking the syringe to release air bubbles, poking the jab into bared arms. Men several spots back in the line bunched their sleeves up onto their shoulders in cooperative anticipation – with such ambitious targets, the gesture seemed to suggest, no efficiency was too small to count. “We are doing everything we can to succeed in this campaign,” said Dr Ayesha Akhter, assistant director of the hospital and its COVID-vaccination focal point. “We see thousands of people coming to the hospital every hour.”

Credit: Gavi/2022/Saydul Fateheen Murad
Several kilometres to the west in industrial Savar, a health-complex hall sounded, by mid-afternoon, like a thronged railway station: chatter echoed off the fan-studded ceiling, feet shuffled, paper rustled, and a megaphone crackled out announcements. Elsewhere in Savar, home to millions, the energetic response to the mega campaign would slide at moments towards chaos – scuffles in the crowd were reported at at least one of the area’s 20 vaccination points.
But crucially, it would also result in significantly increased protection from future infection for the population of the densely-inhabited district. Dr Saymul Huda, a health inspector and family planner from the locality said: “In Savar, there is no way to stop the vaccination. We have two million workers in our city – if we stop, then a lot of people will be left out of vaccination.”
He recalled the terrible first wave of COVID-19 – the ranks of volunteer health workers being trained in a hurry, the bodies nobody wanted to touch to bury. “I feel that for Bangladesh vaccination is so important,” he said. During the most recent surge, Savar saw high case counts but no fatalities, “so we understand that COVID vaccines are working well.”
By Saturday evening, the government had called for a two-day extension to the mega campaign. Two days later, when the campaign wrapped up, the tally of new vaccines delivered stood at a staggering 12 million, bringing the portion of Bangladesh’s population to have received a vaccine up to 72%. The proportion who qualified as fully immunised against COVID-19 now stood at 49%.

Credit: © UNICEF/UN0491062/Sujan
In many parts of the world, declining rates of severe and fatal COVID-19 – largely a result of increased vaccine protection – have seemed to usher in a period of lagging vaccine uptake, even as blockages in global vaccine supply chains have finally eased.
“As the disease burden continues to decrease around the world, risk perception will surely be low, leading to less concern and [lower emphasis on] importance of vaccination in many parts of the world – including Bangladesh,” says Robert Kanwagi, Demand Generation Lead for Gavi.
In other words, declining vaccine demand amid lower rates of illness is not a pattern that Bangladesh is inherently exempt from. On the contrary, a 2021 paper co-authored by Kanwagi and published in the scientific journal PLOS ONE, found that in Bangladesh, beliefs about the risk of getting COVID-19 were predictive of vaccination uptake.
Have you read?
Specifically, vaccine “acceptors” were 1.4 times more likely than “non-acceptors” to say it was “very likely” that someone in their household would get COVID, 1.3 times more likely to say they were “very concerned” about getting infected, and 1.3 times more likely to say it would be “very serious” if someone in their household got ill. Put simply, feeling more worried about COVID made Bangladeshis more willing to go and get the jab.
“It’s about hierarchy of needs – what is the most needed thing/item now? Is it the vaccine? Or income/work?” Kanwagi wrote in a message. “Unless you mobilise and continue to drum the importance and existence of vaccines, we risk seeing low uptake even in countries with high willingness.”
That’s understandable, but given the continuous evolution of the pandemic, vaccination remains the best way to stay safe against whatever COVID-19 may bring in the future. Science says that a next new variant is around the corner, and that it could be more severe. So how can governments activate their unvaccinated or part-vaccinated constituents to go out and seek the jab, even when the danger seems to be ebbing? Bangladesh’s approach – condensing a high number of vaccinations into a short period of time with considerable fanfare – clearly has merits.
“Mass vaccination solves two key barriers – ease of geographical access and favourable timing, but also positive peer influence. Peers are likely to get vaccinated once they see their colleagues get vaccinated,” says Kanwagi. Bangladesh’s February mega-campaign was conducted across more than 30,000 vaccination booths.
In fact, large vaccination events like February’s have punctuated Bangladesh’s vaccination drive since last year. In August, after international supply constraints loosened, unhobbling the Bangladeshi vaccine plan, a five-day mass drive built momentum. In September, Prime Minister Hasina’s birthday became an occasion for a drive aiming to broaden protection to 7.5 million further vaccinees.
“Bangladesh didn’t necessarily reach the 40% global target by the end of 2021. This was due to the fact that there was a global supply shortage,” clarifies Nilgun Aydogan, Gavi’s Bangladesh country manager. “However, mass campaigns supporting the national implementation plan brought them very close to the target at the end of the year.”
Now, the country has its sights set on the WHO’s 70% full-vaccination target by mid-year. It’ll take a bit of a push: after a second-round campaign in late March, approximately 57% of Bangladesh is double-dosed – and Ramadan in April may slow the vaccine rollout’s pace somewhat.
Will Bangladesh achieve its summer goal? Hard to say for certain. But if it doesn’t, it won’t be for lack of dedication. “One of the elements that’s unique about Bangladesh is their commitment,” says Aydogan. “There has always been a commitment to immunisation from the government, all the way from the Prime Minister’s level… and they’ve really been going the extra mile for COVID.”