Long mpox? Research suggests mpox may cause health problems long after the rash heals
Study finds scarring plus bowel, urinary and sexual problems more than a year after clade II mpox infection.
- 20 January 2026
- 5 min read
- by Linda Geddes
At a glance
- During the 2022–2023 global mpox outbreak, clinical focus was largely on the immediate illness – painful rashes, fever and occasional hospitalisation – with little known about longer-term effects.
- A new study published in Annals of Internal Medicine assessed 154 people infected with clade IIb mpox 1–-18 months after diagnosis. Fifty-eight percent of them had at least one lasting physical effect, most often scarring, while 13% reported ongoing problems such as bowel or urinary control issues, or persistent sexual dysfunction.
- The findings suggest mpox is not always a short-lived illness. Longer-term follow-up may be needed, including dermatological, sexual health and psychosocial care, alongside continued efforts to prevent infection.
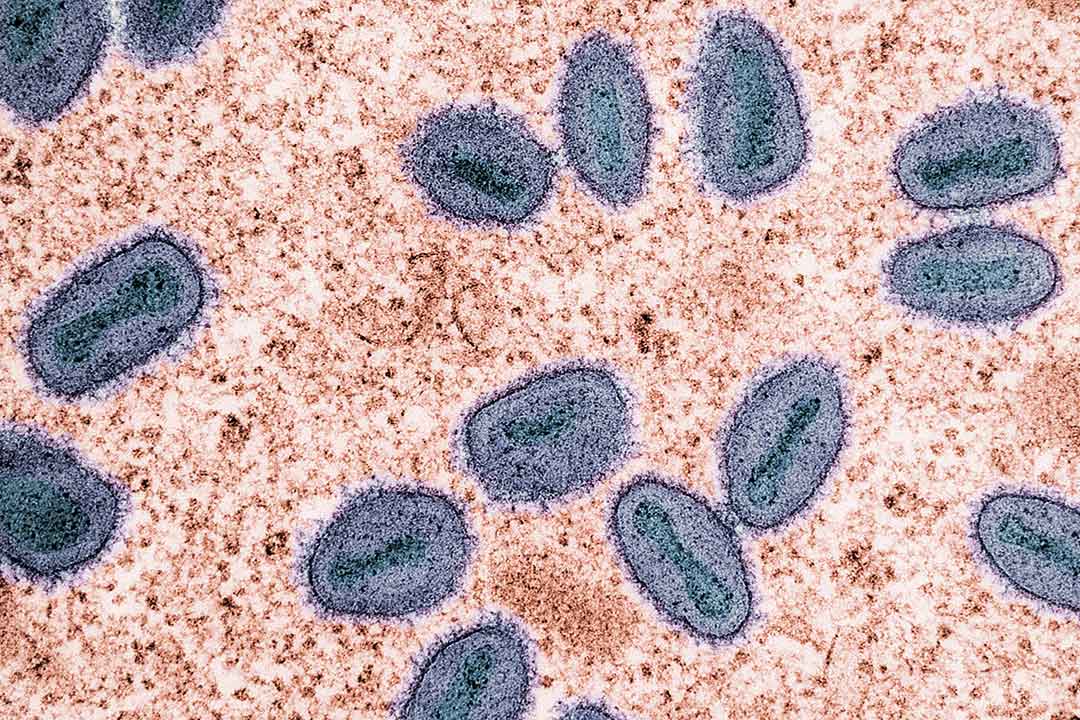
Mpox is rarely subtle. The illness can begin with fever and exhaustion, but it is the rash that people remember: painful, blistering lesions that can spread across the body, often concentrating on the genitals and anus, and sometimes the face.
For some patients during the 2022–2023 mpox outbreak, the pain was so severe that sitting, urinating or sleeping became ordeals, and hospital care was required.
Until recently, the prevailing assumption was that once the rash healed, the worst was over. But new research suggests that for a substantial minority, mpox does not end when the scabs fall away.
A year or more after infection, a substantial proportion are still living with physical scars – and, in some cases, lasting problems with bowel, bladder and sexual function.
The 2022–2023 mpox outbreak was caused by a strain of the virus known as clade IIb mpox and spread largely through close physical contact, particularly among men who have sex with men in countries where mpox was not previously endemic.
By the time the World Health Organization declared the end of the public health emergency in May 2023, more than 87,000 cases and 140 deaths had been reported from 111 countries.
The prevailing assumption was that once the rash healed, the worst was over. But new research suggests that for a substantial minority, mpox does not end when the scabs fall away.
What are the longer-term consequences of mpox infection?
Dr Preetam Cholli and the US Centers for Disease Control and Prevention (CDC) and colleagues set out to investigate the longer-term effects of mpox on people’s physical appearance and broader health.
They assessed 154 US adults who had been diagnosed with mpox between May 2022 and January 2023, conducting surveys and physical examinations 11–18 months after infection, and compared the results with 201 adults at similar risk of mpox who had never been infected.
The research, published in Annals of Internal Medicine, found that 58% of those who had mpox were left with at least one lasting physical effect, most commonly scarring at the sites where lesions had healed.
This included the penis and surrounding skin, the groin and pelvic region, the face and ears, and the trunk and upper limbs. Most people had fewer than ten scars, typically clustered in one or two areas of the body.
But physical appearance was only part of the story. Thirteen percent of people reported ongoing functional problems, including difficulty with bowel movements, urinary symptoms, chronic pain and, in a small number of cases, neurological or visual impairment.
18% reported either losing their job because they contracted mpox or having to change their job because of the inability to do the same work after mpox, whereas 8% reported being refused employment because of having had mpox.
Ongoing difficulty defecating or stool incontinence was the most reported issue, affecting roughly 6.5% of individuals (10 of 154), followed by urinary hesitancy or incontinence, which affected 4.5% of them (7 of 154).
Even so, nearly nine in ten post-mpox patients rated their overall health as good, very good, or excellent when they were evaluated, and only a few had ongoing health needs, such as needing mobility aids, or relying on physiotherapy or mental health support services.
On the other hand, longer-term social impacts were common: nearly half said mpox was still affecting their social lives, one in five reported ongoing sexual difficulties and six percent said it had affected their work.
“Some post-mpox participants reported experiencing mpox-related stigma: 30% felt hurt by how people reacted to their mpox diagnosis, and 22% reported other people were hesitant to be around them since their diagnosis,” the researchers said.
Have you read?
“In addition, 18% reported either losing their job because they contracted mpox or having to change their job because of the inability to do the same work after mpox, whereas 8% reported being refused employment because of having had mpox.”
Those with persistent scarring or skin discolouration were more likely to report ongoing, negative impacts on their social lives than those without, while those with continuing physical problems were nearly five times more likely to report sexual issues.
What do these findings mean for people recovering from mpox?
Mpox remains a public health concern. In 2024, WHO declared a public health emergency of international concern in response to a sharp rise in cases in the Democratic Republic of the Congo and neighbouring countries, linked to the clade I form of the virus.
Although that emergency designation was lifted in September 2025 as cases declined, “the outbreak has prompted calls for research into the long-term sequelae of clade I mpox,” the researchers said. They noted that while their study focused on clade IIb mpox, the findings still offer valuable insights into the types of lasting physical and psychosocial effects the virus can cause.
Meanwhile, clade IIb – the strain behind the 2022–2023 global outbreak – continues to circulate at low levels in many countries, causing sporadic cases but no longer driving large international outbreaks.
These latest findings suggest that mpox is not always a short-lived illness. The authors say some patients may benefit from longer-term follow-up, including care for skin scarring, sexual health problems and psychosocial impacts, alongside continued efforts to prevent infection.








