Vaccine profiles: Typhoid
Typhoid is rampant in countries with poor water, sanitation, hygiene and food safety, and the bacterium is developing resistance to almost every antibiotic available. This means that rolling out the typhoid conjugate vaccine is more urgent than ever.
- 11 January 2023
- 6 min read
- by Priya Joi
In today's pandemic parlance, Mary Mallon would probably be dubbed a typhoid 'superspreader'. Indeed, the ability of 'Typhoid Mary' to cause several outbreaks of typhoid in New York City where she worked as a cook in the early 20th century, is where the idea of highly contagious disease carriers came from.
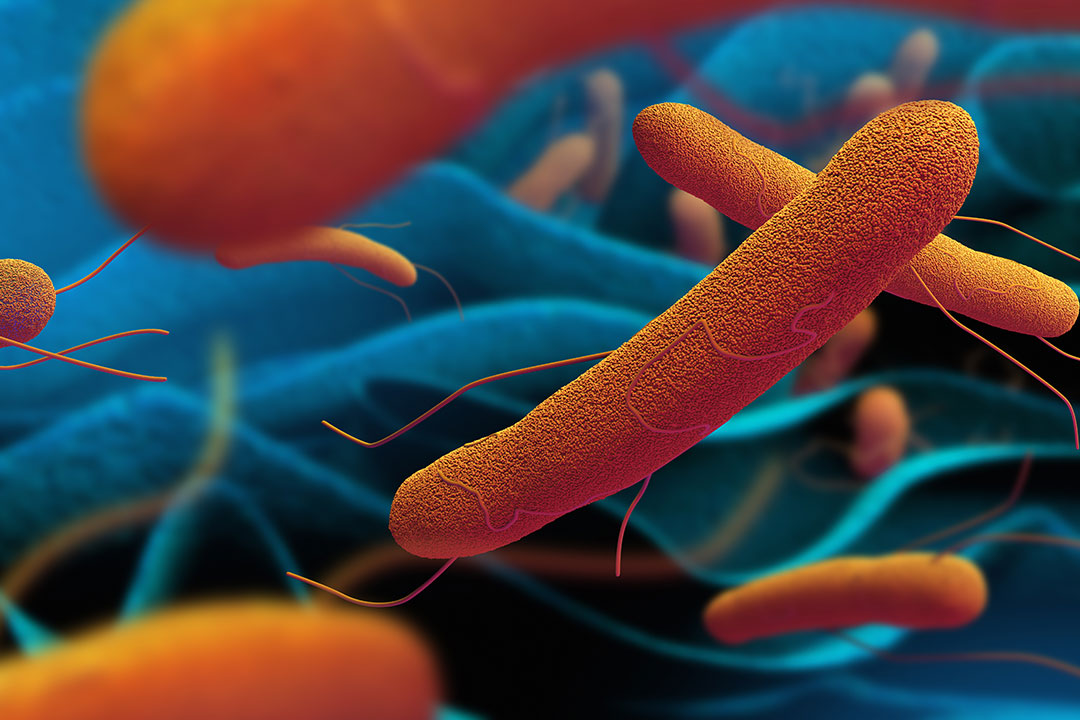
Typhoid is a bacterial disease caused by Salmonella typhi that infects the intestinal tract and bloodstream; it is spread when water or food supplies are contaminated by faeces containing the bacterium. The symptoms are a high and persistent fever, diarrhoea or constipation, stomach pain or a headache.
In many countries where typhoid is still a public health threat, inadequate water and sanitation infrastructure can combine with unpredictable rainfall and flooding to create the perfect storm for an outbreak of typhoid. Countries like Pakistan and Zimbabwe have responded to typhoid outbreaks by leading the charge in using typhoid vaccines.
Mary Mallon infected so many family members in households that she worked in that she was publicly demonised as a 'walking typhoid fever factory' and sent into isolation in North Brother island, a prison isle in New York's East River, for a quarter of a century until she died there, alone.
Had she been born a few decades later, her life would have turned out very differently. The first vaccine against S typhi was developed in 1896, but it was not used extensively until wars and the ability of infectious diseases to spread faster made the vaccine valuable and it became more widely used from 1911. Antibiotics became available in 1948.
Spreading through poor hygiene
Infectious diarrhoea and dysentery were described so clearly in Hippocrates' aphorisms that medical historians think typhoid fever has been around since his time.
Since then, it has ravaged societies where there is less ability to ensure the hygiene of food and water supplies. In North America and Europe, there was high transmission of typhoid fever from the 19th century until the early 20th century.
Then the development of a vaccine and antibiotics as well as the expansion of water and sanitation systems and public health practices such as handwashing – which Typhoid Mary didn't practise – along with improved food safety, massively reduced the spread of waterborne and foodborne diseases such as typhoid, and others such as cholera.
While this incidence of typhoid fell in countries where water access, sanitation, hygiene and food safety improved, it remains a major public health challenge in low-income countries and communities, where those are inadequate. One in three people in the world, mostly in low-income countries, still don't have access to a toilet. Typhoid still makes up to 20 million people sick and kills up to an estimated 161,000 every year.
Have you read?
In many countries where typhoid is still a public health threat, inadequate water and sanitation infrastructure can combine with unpredictable rainfall and flooding to create the perfect storm for an outbreak of typhoid. Countries like Pakistan and Zimbabwe have responded to typhoid outbreaks by leading the charge in using typhoid vaccines.
As Salmonella typhi only lives in humans and has no animal host, nor does the bacterium live outside people, improving water,sanitation, hygiene and food safety can have a dramatic effect in halting disease transmission.
Vaccine development
The first typhoid vaccine was developed in 1896 by British and German scientists Almroth Edward Wright, Richard Pfeiffer and Wilhelm Kolle. It was a heat-killed, whole-cell S typhi vaccine.
Two vaccines have been in use for years – an injectable vaccine based on the purified antigen for people aged over two years and a live attenuated oral vaccine in capsule formulation for those aged over five years. However, neither can be used in children younger than two years and they do not provide long-lasting immunity. The injectable vaccine needs a booster after two years, and the oral vaccine requires a booster after five years. Uptake of the vaccine had been low because of this.
The growing inability in some regions to treat typhoid effectively emphasises the need for widespread vaccination with TCV in high-risk areas to reduce the incidence of disease and slow the spread of drug-resistant typhoid.
Then in 2017, WHO prequalified a new protein-conjugated typhoid vaccine (TCV), that not only had longer lasting immunity but could be used from six months of age. Gavi began funding the rollout of TCV into national routine immunisation schedules, along with a catch-up campaign for those up to age 15, in countries with high typhoid burden as well as those at risk of the spread of antimicrobial resistant typhoid.
Momentum is building for new countries to introduce TCV, and coverage has slowly been increasing in countries that already introduced, although some campaigns – such as the final phase of the rollout that took place a few months ago in Balochistan, Pakistan – had been delayed by the COVID-19 pandemic. That it took place at all given the extreme flooding the country was facing was a testament to the determination of local health staff, who knew that the risk of typhoid would spike following heavy rain.
Extreme antibiotic resistance
First-line antibiotics used to treat typhoid were chloramphenicol, ampicillin, and cotrimoxazole, though resistance first appeared in the 1970s and has spread. Today we face the global spread of multi-drug resistant (MDR) typhoid, especially in the Middle East, Africa and Asia.
In response to this growing resistance, another class of antibiotics called fluoroquinolones began to be used in the 1990s, though widespread use meant that resistance began rising to this class of drugs as well. As a result, cephalosporins and azithromycin began to be used as last resort antibiotics.
Worryingly, extremely drug-resistant (XDR) typhoid strains were identified in 2016 that were resistant to five classes of antibiotics: chloramphenicol, ampicillin, cotrimoxazole, streptomycin, fluoroquinolones and third-generation cephalosporins. Only azithromycin is still effective in treating XDR typhoid patients, and azithromycin resistance is now also emerging in some geographies. This is creating a dire situation in which the complexity and cost of treatment is increasing, and more people may need to be hospitalised for their care, straining health systems.
The growing inability in some regions to treat typhoid effectively emphasises the need for widespread vaccination with TCV in high-risk areas to reduce the incidence of disease and slow the spread of drug-resistant typhoid. Effective rollout of the TCV vaccine would prevent two-thirds of cases and deaths, and the proportion of typhoid cases that are drug resistant could decrease by more than 16% in Gavi-supported countries over a decade with appropriate vaccine rollout.