Vaccine profiles: Ebola
Vaccines against Ebola virus have transformed our ability to tackle outbreaks, but further vaccines and interventions are urgently needed.
- 15 April 2025
- 10 min read
- by Linda Geddes
West Africa still bears the scars of the Ebola outbreak that erupted there a decade ago.
With more than 28,600 cases and 11,323 deaths, many people in hard-hit areas of Sierra Leone, Guinea and Liberia know of someone who lost a loved one, if they didn’t lose someone themselves.
The tension and anxiety that permeated everyday life, with harsh curfews and quarantines, is also hard to forget.
Interviews conducted with survivors in Calabra Town, Sierra Leone, during 2016 and 2017 bear witness to some of the daily challenges that people faced:
“Everything was difficult. You cannot move, and if you cannot move, you cannot work. And if you don’t work, you don’t have money. And if you don’t have money, you cannot buy food,” a 50-year-old teacher said.
“[Ebola] ravaged the whole country. A lot of nurses died, doctors died, lay people died. And because of that, when it was here, we were afraid of each other,” added a 53-year-old nurse.
“We cried a lot because seeing a colleague dying, seeing a member of your family dying, seeing a friend dying, seeing a relative dying, and you can’t do anything. You can’t touch them, you can’t bury them, you know it was terrible.”
Deadly outbreaks
Between 2014 and 2016, Sierra Leone, Guinea and Liberia experienced the largest Ebola outbreak since the virus was first discovered in 1976.
It was by no means the last: since then, further outbreaks have hit Guinea, Uganda, and the Democratic Republic of the Congo (DRC) – including a massive outbreak that claimed at least 2,287 lives in DRC between 2018 and 2020. As this article was being written, Uganda was fighting an outbreak of Ebola caused by Sudan virus, which had claimed at least four lives.
The good news is that vaccines against Ebola virus – the pathogen responsible for the 2014–16 and 2018–20 outbreaks – have since been licensed and emergency stockpiles developed.
“All Ebola outbreaks that have occurred since we had a stockpile were quickly stopped – thanks to the vaccines and rapid other response measures,” says Allyson Russell, an epidemiologist and senior programme manager in Gavi’s High Impact Outbreaks team.
However, these vaccines aren’t effective against the other three orthoebolaviruses that cause Ebola disease in humans – including Sudan virus.
A trial of a Sudan virus vaccine candidate has just been launched in Uganda, but the unpredictability and fast-moving nature of Ebola outbreaks makes testing vaccine efficacy difficult, says Russell.
Besides vaccines, more work is also needed to build the infrastructure to deliver them, and forge partnerships with Ebola-affected and at-risk communities, to ensure that outbreaks are swiftly spotted, and public health measures implemented to limit their spread.
Ebola basics
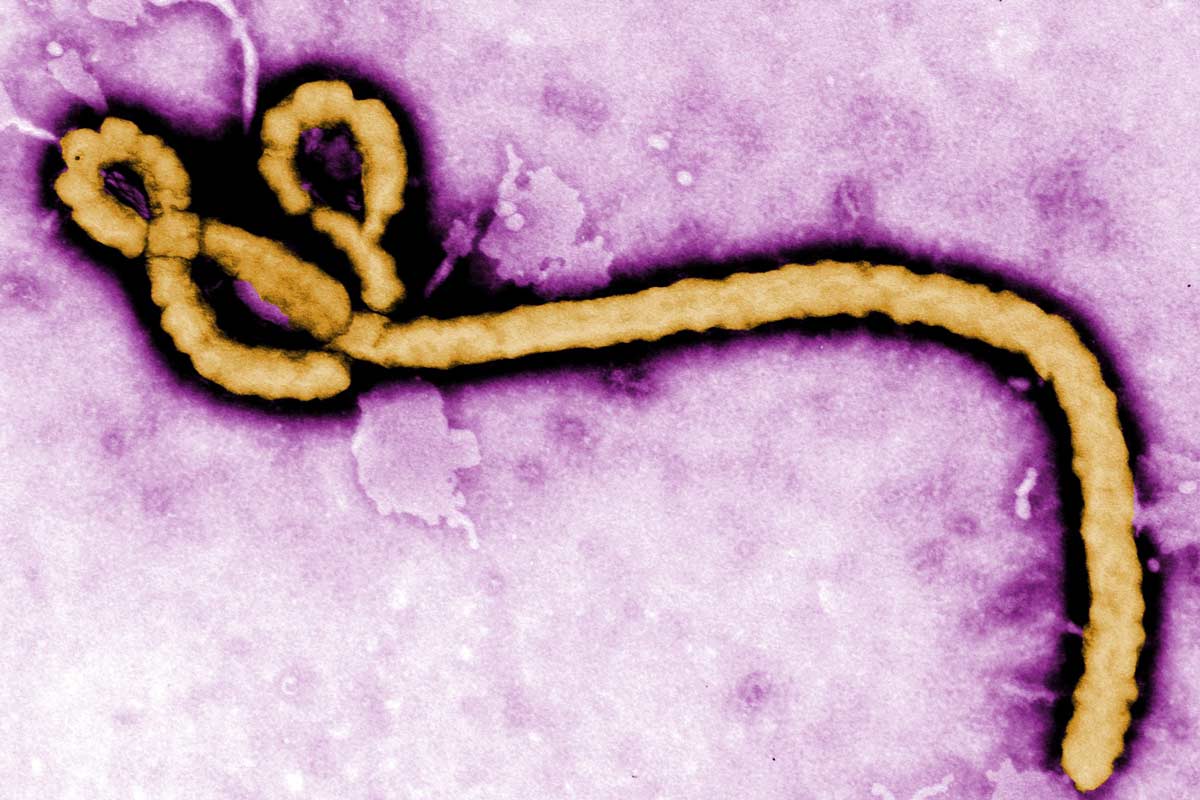
Ebola virus disease is a severe illness affecting humans and other primates. Transmitted to people from wild animals, and then spreading from person-to-person through direct contact with body fluids, or surfaces and material contaminated with these fluids, Ebola’s fatality rate of between 50% and 90% commands understandable fear and attention.
The virus can also linger in a small number of survivors, occasionally resurging and triggering further infections. Though rare, this makes monitoring the health of Ebola survivors and supporting their recovery critical.
People aren’t usually infectious until they develop symptoms, typically eight to ten days after becoming infected themselves. These usually begin with fever, fatigue, muscle aches, headaches and a sore throat, followed by diarrhoea, vomiting, rashes and issues with their kidneys or liver.
Ebola’s fatality rate of between 50% and 90% commands understandable fear and attention.
Some people also experience internal or external bleeding, for instance from their gums or rectum.
Treatment includes supportive care to keep people hydrated and maintain their blood pressure and oxygen levels, as well as medication to manage fever, pain, vomiting and diarrhoea.
Two monoclonal antibodies are recommended for the treatment of Ebola virus disease, but these don’t work against other causes of Ebola, such as Sudan virus.
Vaccine development
Ebola was first recognised in 1976 following an outbreak of Ebola virus in what is today known as DRC.
Efforts to develop a vaccine against this pathogen quickly followed, but because early outbreaks tended to be small and quickly contained, there was little commercial incentive to invest in vaccine development.
Even so, recognising the potential biosecurity risk of Ebola being weaponised and deliberately released, several national defence agencies continued to research potential Ebola vaccines and treatments, including the USA and Canada.
These efforts intensified following the 9/11 terror attacks, and by the time the West Africa outbreak of Ebola struck in 2014, ten Ebola vaccines and treatments were in various stages of development and testing.
In August 2014, the World Health Organization (WHO) declared the outbreak a Public Health Emergency of International Concern – the strongest global alert that it can formally make – to trigger action from global partners.
According to a study that investigated the real-world effectiveness of the vaccine during the 2018–2020 Kivu Ebola epidemic, it was 84% effective against Ebola virus disease.
At that time, one of the most advanced candidates was the rVSV-ZEBOV vaccine, which had been developed by Canada’s National Microbiology Laboratory, and which uses a weakened livestock virus called vesicular stomatitis virus (VSV) to deliver the gene for an Ebola virus protein into human cells, triggering an immune response.
Canada’s federal government donated doses of this vaccine for use in West Africa and licensed its manufacture to NewLink Genetics and Merck Sharpe & Dohme (known as Merck in the US and Canada).
In 2015, a clinical trial of the vaccine began in Guinea, with around 12,000 people eventually vaccinated as part of a ‘ring vaccination’ strategy – where every contact of a suspected case, plus the contacts of those contacts, is offered the vaccine.
The measured efficacy at that time was 100% (with a calculated lower confidence interval of 68.9%). Trials of several other Ebola vaccines also began at around the same time, including the Ad26.ZEBOV and MVA-BN-Filo vaccines developed by Johnson and Johnson.
Meanwhile, efforts to commercialise an Ebola vaccine were bolstered by Gavi, the Vaccine Alliance, which offered manufacturers with vaccine candidates in clinical trials a prepaid commitment to buy doses of licensed vaccines, as and when they became available.
Merck and Gavi subsequently executed an Advance Purchase Commitment in January 2016, which meant that doses of rVSV-ZEBOV vaccine would be available for use in outbreaks in the context of clinical trials, even before it had been fully licensed by regulators.
Since 2021, a Gavi-funded global emergency stockpile of 500,000 doses of the rVSV-ZEBOV vaccine has been accessible worldwide. It is available to all countries for outbreak response.
Drawing upon this supply of investigational vaccines became necessary in 2018, when DRC was hit by two separate outbreaks of Ebola – the second affecting the Kivu region of Eastern DRC and spiralling into what became the second largest outbreak in history.
Although at least 2,299 people died during the Kivu Ebola epidemic, the vaccine was credited with preventing the loss of further lives and slowing the spread of Ebola.
Recognising the importance of rapid access to doses in such emergencies, in late 2019 Gavi announced that it would fund a global emergency stockpile of Ebola vaccines that would be available to all countries for outbreak response and prevention. This stockpile was launched two years later.
Current Ebola vaccines
This launch was possible thanks to the rVSV-ZEBOV vaccine receiving WHO prequalification – meaning it meets international standards for quality, safety and efficacy – in November 2019.
It is designed to be given as a single dose and is currently recommended for reactive ring vaccination during outbreaks, and can also be used preventively to vaccinate health and frontline workers in at-risk areas. According to a study that investigated the real-world effectiveness of the vaccine during the 2018–2020 Kivu Ebola epidemic, it was 84% effective against Ebola virus disease in individuals vaccinated at least ten days before exposure.
Johnson and Johnson’s Ad26.ZEBOV and MVA-BN-Filo vaccine regimen, sold under the brand names Zabdeno and Mvabea, received WHO prequalification in May 2021. It is designed to be give as two doses, 56 days apart.
The first dose uses a modified and harmless adenovirus to deliver the genetic code for an Ebola protein into human cells, triggering an immune response. The second dose uses a weakened strain of the vaccinia virus used in smallpox and mpox vaccines to deliver a different Ebola protein into human cells.
Although the real-world effectiveness of this vaccine is not yet known, a study published in The New England Journal of Medicine in 2022 confirmed that the vaccine was safe and triggered durable immune responses, with antibodies still detectable a year after adults and children received their first doses.
Because of the delay between the doses, this regimen is currently recommended for people who are at moderate risk of Ebola but are not considered to be at high risk – such as preventively in laboratory workers who may be exposed to Ebola virus disease, or health workers in areas with historical Ebola outbreaks.
Ebola vaccine stockpile
Since 2021, a Gavi-funded global emergency stockpile of 500,000 doses of the rVSV-ZEBOV vaccine has been accessible worldwide. It is available to all countries for outbreak response following a request to the International Coordinating Group on Vaccine Provision, which manages the stockpile.
Gavi-eligible low- and lower middle-income countries can access the stockpile free of charge and receive support for operational costs associated with delivering this vaccine into people’s arms.
“It is critical that we maintain the stockpile for future outbreaks and health security,” says Russell. “Meanwhile, during periods where there are no outbreaks, we aim to make efficient use of the stockpiled vaccines to preventively vaccinate at-risk frontline workers and be better prepared for the next outbreak.”
In June 2024, Gavi announced that the lower-income countries it supports could apply to access Ebola vaccines to preventively vaccinate frontline and health workers in at-risk countries. This followed a decision by the WHO’s Strategic Advisory Group of Experts on Immunization (SAGE) to officially recommend the use of the rVSV-ZEBOV and Zabdeno/Mvabea vaccines for preventive use in populations at high risk of being exposed to Ebola through their duties as frontline care providers and in response to outbreaks.
Have you read?
Future challenges
Despite these vaccines, challenges remain. Further research is needed to understand the duration of protection afforded by vaccines, although a recent study indicated that the immunity conferred by the rVSV-ZEBOV vaccine remains high five years after vaccination.
Another challenge is the absence of a vaccine against other types of Ebola-causing virus – particularly Sudan virus, which has caused nine human outbreaks in Sudan and Uganda since its discovery in 1976.
Like Ebola virus, it has a high case fatality rate, ranging from 41% to 70% in past outbreaks, and causes similar symptoms. However, even though these viruses share many similarities, they have different genetic material and different proteins which means that different vaccines are needed for each species.
Several vaccine candidates against Sudan virus are being developed, including some that have already entered clinical trials.
One of these candidates, developed by the International AIDS Vaccine Initiative (IAVI), uses the same rVSV viral vector platform as the ERVEBO vaccine, but encodes a surface protein from Sudan virus, rather than Ebola virus.
It is currently being evaluated in a ring vaccination trial as part of the public health response to the current outbreak of Sudan virus disease in Uganda. Also needed are additional drugs against this and other types of Ebola virus disease.
“Critical to the success of Ebola vaccination activities is effective engagement and collaboration with healthcare workers and communities to ensure they have the right information about the vaccine, its risks and benefits, and can be advocates themselves in their networks and communities,” says Russell.
Game-changing as vaccines are, they are also only part of a package of interventions needed to stem outbreaks.
A key insight from the 2014–16 West Africa epidemic was the need to build trust in communities affected by Ebola, where fear, misinformation and mistrust of vaccines and/or health workers may be rife. Disease surveillance and public health messaging about how to avoid spreading the virus are difficult to implement without building these relationships.
Progress against Ebola has come a long way since the virus was first discovered almost 50 years ago. But the threat it poses hasn’t gone away; since 1994, the frequency of Ebola outbreaks has notably increased, and some experts are concerned that large outbreaks may be becoming more commonplace.
As the West Africa outbreak demonstrated, Ebola is an extraordinarily destructive disease. An extraordinary effort is needed to stop it wrecking further havoc on people's lives. Yet, through improved surveillance, tracing the contacts of infected individuals and vaccines, it is possible to stop outbreaks before they spread.
More from Linda Geddes
Recommended for you








