
Dagfinn Høybråten
Board Chair of the GAVI Alliance
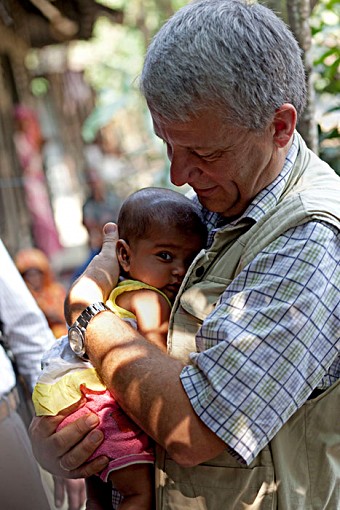 As I chair the GAVI Alliance Board meeting in Bangladesh and discuss decisions that will shape the future of immunisation in the developing world, it will be important to remember health worker Rabbi Aztor who I met on a field trip earlier this week.
As I chair the GAVI Alliance Board meeting in Bangladesh and discuss decisions that will shape the future of immunisation in the developing world, it will be important to remember health worker Rabbi Aztor who I met on a field trip earlier this week.
It is people like Rabbi who fulfill the GAVI mission every single day: delivering vaccines through a weekly ‘Vaccination Day’ held in the living room of her home at Bara Goan, a village set 55km south of Dhaka amid the tributaries of the Padma river.
I watched as mothers waited patiently for Rabbi to register the weight, height and health of their newborn babies. Her measurements complete, she pulls life-saving vaccines out of a cold box.
This morning it is 10-week-old Fatema’s turn. Like children across the world, she cries as Rabbi drops rotavirus vaccine into her mouth and administers a second dose of pentavalent vaccine. Her mother Maksuda Aketer, aged 41, looks on calmly: she has already seen Rabbi deliver the same vaccines to her two elder daughters and knows this simple five-minute act will offer life-long protection against the biggest child killers in Bangladesh: diarrhoea and pneumonia.
Immunisation sessions like these are held once a week at Rabbi’s house. In between, the health worker makes daily calls on the community’s young babies to check on progress and ensure mothers do not forget immunisation schedules.
Rabbi says that during the monsoon season, when Bangladesh’s rivers can flow four metres above their normal depth and local homes become small islands perched on raised embankments, Rabbi uses a small paddleboat to reach her patients.
Rabbi works for the International Centre for Diarrhoeal Disease Research, Bangladesh (icddr,b), the medical centre based at nearby Matlab, whose pioneering research has laid the foundations for Bangladesh’s routine immunisation rates to reach an astonishing 95% of infants.
Forty years ago, icddr,b successfully piloted the concept of Bangladeshi health workers deliberately selected from the local community to ensure they have the trust and respect of their neighbours. Today 46,000 trained health workers underpin the nation’s maternal and child health programme.
 This is just one example of iccdr,b pushing back the boundaries of public health in developing countries.
This is just one example of iccdr,b pushing back the boundaries of public health in developing countries.
The centre’s medical and demographic surveillance programme has been running for almost 50 years: the longest running in the developing world.
Ever since a group of scientists conducted research on a cholera vaccine in the early 1960s, based on a boat in the Padma River, icddr,b has monitored the health and welfare of some 220,000 people – from cradle to grave.
Three generations of local villagers have grown used to icddr’s surveys, with studies ranging from the impact of new vaccines against influenza and pneumococcal disease to the reasons why drowning is the number one cause of death among young children in Bangladesh.
The rotavirus vaccines that Rabbi is administering are part of an impact assessment study funded by GAVI.
Round the corner from Rabbi’s house, I watch as another villager uses a handheld PDA to input data about the health of a newborn child; the information is fed via satellite into a giant database back at iccdr,b’s centre in Matlab.
Later in the day, I am taken by motor launch down the Padma, navigating fishing boats and brightly coloured water hyacinths, to Matlab to see the result of this research: a library of yellowing folders and a state of the art database that contains information about four generations of Bangladeshis.
Scientists from international medical schools around the world, such as the London School of Tropical Medicine in London and the Johns Hopkins University regularly consult the medical equivalent of an oracle.
Matlab runs its own hospital, and as I meet the staff and patients I am reminded of the need of the vaccines that Rabbi administered to Fatema earlier in the day.
On one side of the hospital’s courtyard, I visit a ward for newborn babies suffering from diarrhoea – the doctor explains that it is approaching the peak season for diarrhoea cases in Bangladesh and most of the beds are already taken-up.
On the other side, a 17-day-old baby in the neonatal clinic wheezes gently and snuggles deeper into the comfort of her mother’s arms – she has contracted pneumonia. Thanks to Matlab’s amazing medical care and antibiotics, she will survive.
Diarrhoea and pneumonia – Bangladesh’s (and the developing world’s) number one killers of infants. Both are vaccine-preventable diseases: rotavirus vaccine for diarrhoea, pneumococcal vaccine for pneumonia.
Bangladesh has applied for GAVI funding for the introduction of these vaccines, with pneumococcal vaccine support set for approval in 2012.
As we focus on points of order and policy decisions at the GAVI Board this week, we should keep in mind what it is all about: health workers like Rabbi who need GAVI support to continue to do their job on the frontline of immunisation.
