Discussion Paper
April 2023
Contents
Building a framework for early pandemic response
Working together to achieve common goals
Disclaimer:
This document is published by Gavi, the Vaccine Alliance.
The contents included is the result of a collaborative process managed by Gavi. The republication or usage of the content of this document of any kind without written permission is prohibited. Please contact media@gavi.org with any requests for use.
Share
Introduction
The H1N1 pandemic of 2009 infected an estimated 11-21% of the global population.1 For Ebola outbreaks, case fatality rates vary widely but have reached as high as 70%. Most people with the Zika virus do not develop symptoms, yet it can cause brain defects in babies. Those aged 60 and over are hundreds of times more likely than children to die from COVID-19.2
The last 20 years has demonstrated just how diverse infectious diseases outbreaks, epidemics and pandemics can be. They can spread locally or regionally, affect young and old differently, and can come at a huge cost, both in terms of the tens of millions of lives affected and the local or global economic damage. Recent research suggests that environmental changes may drive a doubling of the frequency of severe pandemics in the coming decades.3
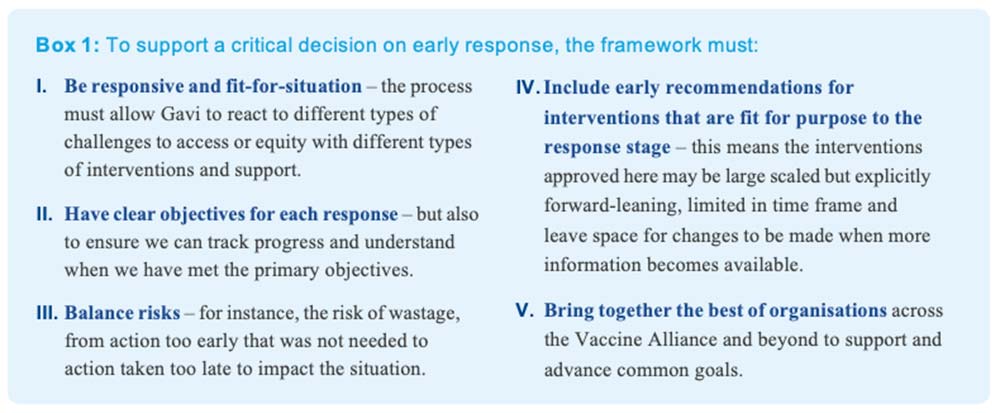
This diversity of threats can make it difficult to know how best to respond. There are no risk-free approaches. Waiting for certainty and perfect solutions will likely result in acting too late, while early action can save lives and cost considerably less than the long-term economic impact. Decisions about what to do must be rapid and factor in the information available, even if incomplete and highly uncertain. That's why, as part of broader pandemic prevention, preparedness and response (PPPR) efforts, Gavi is working with Alliance and other partners to develop an emergency response decision-making framework for outbreaks of pandemic potential, to ensure the world is ready to respond rapidly to future threats, with clear operational plans and defined roles and responsibilities.
This discussion document lays out the in-progress design framework. It provides specific comments on how the framework and its associated triggers link to the role and need for emergency interventions and the need to unlock critical contingent financing.4 The purpose is to engage partners, including country-based experts, early in the framework-building process, and facilitate coordination with other organisations and their respective decision-making tools.
Since it was created in 2000, Gavi has helped to vaccinate more than one billion additional children and prevented more than 16.2 million deaths in lower-income countries through routine immunisation (RI). In addition to protecting the lives of vulnerable children through RI, Gavi plays a vital ongoing role in PPPR.
First, Gavi helps build stronger and resilient primary health care systems, which are vital for disease surveillance and pandemic response. Second, Gavi provides funding to support vaccine stockpiles to help manage outbreak response for diseases like yellow fever, Ebola, cholera, meningitis, and others. Third, it has created innovative ways to finance immunisation programmes, and to incentivise accelerated vaccine development, production and introduction. For example, in response to the 2014-2016 Ebola epidemic, Gavi worked with manufacturers to incentivise and accelerate the development of early-stage vaccine candidates and signed an Advance Purchase Commitment to help accelerate the first Ebola vaccine through licensure and WHO pre-qualification. This paved the way for the creation of the global stockpile of licensed Ebola vaccine.
With vaccines often one of the best lines of defense in responding to a public health threat, Gavi is a critical partner in pandemic response, at the global, regional, and local levels.
Indeed, building on our experiences and lessons from both our initial response to the COVID-19 pandemic and then through COVAX (refer to https://www.gavi. org/programmes-impact/our-impact/evaluation-studies for forthcoming independent evaluation reports), and with an eye on future outbreaks of pandemic potential, Gavi is working to organise sources of contingency and at-risk funding and enhanced surge capacities for health agencies in advance, and through solutions built on networked global and regional collaboration.
The types of tools and resources needed will depend on the type of threat and nature of that response. Therefore, the proposed decision-making framework is designed to enable coordinated global responses to future outbreaks of pandemic potential that are tailored to the threat's severity and other characteristics.
Building a framework for early pandemic response
There are existing global, regional, and national systems designed to rapidly detect and respond to major infectious disease threats and outbreaks. Nation states have legal obligations to respond promptly when the World Health Organization (WHO) declares a public health emergency of international concern (PHEIC), as advised by the experts on the International Health Regulations (IHR) Emergency Committee, for example. During such times, Gavi carefully considers guidance from the WHO – its partner in the Alliance. The proposed decision-making framework will complement Gavi's existing health emergency processes and structures to help Gavi ascertain how best to respond, building on its core mission and comparative advantage to invest in providing equitable access to vaccines to save and improve lives, especially in the world's poorest countries.
Building on its existing PPPR work, Gavi is developing this decision-making framework grounded on a set of core principles, including equitable access to vaccines, evidence- based and country-guided decision-making, and leveraging partner immunisation expertise to achieve common goals.
During the early stages of an outbreak when disease progression and country needs are most uncertain it is important that the response be graduated and focused, with a range of interventions (see next section), that enable a timely, early response that can be adapted as more information becomes available – thus the importance of a dynamic framework.
The proposed framework is organised around four steps that define appropriate responses to specific triggers, alongside associated goals, considerations and governance steps:
1. Gavi Engagement
As a first step Gavi Secretariat will rapidly and critically assess whether there are specific and unique contributions to the public health response that require Gavi engagement. Triggers to such an assessment could include report of a local or regional outbreak through to a WHO declaration of a global health emergency. Building on principles from Gavi's Vaccines Investment Strategy (VIS) framework, which is already used for evaluating vaccines for epidemic preparedness and response, an emergency response decision-making framework for outbreaks of pandemic potential will also take into account factors including:
the impact of the threat on routine immunisation; the likelihood of effective disease control through vaccination versus other interventions; and access and equity issues.
2. Recommendations for Action
Proposals for early response are developed based on:
- expert, evidence-informed analysis of the threat and the types of interventions that are most relevant, based on Gavi's engagement with manufacturers and technical agencies;
- experience in innovative financing and vaccine delivery;
- the impact the interventions may have on Gavi's core support to routine immunisation; resource needs;
- and any potential unintended consequences, such as any opportunity costs relating to when a country shifts attention to pandemic response.
3. Initial Response
Recommended initial measures are implemented at-risk to pre-empt escalating needs, but also allow us to collect information to adapt, scale and/or wind-down our response as needed ("Adapted Response") over time. The type of information that Vaccine Alliance partners would consider include shifts in disease epidemiology and risk, any evolution in the role of non-vaccine technologies as part of disease control, changes in the availability of supply or demand for vaccines, and ultimately whether the primary objective of the response was met to inform the next phase of response.
4. Adapted Response Implementation
Next-phase responses are implemented and monitoring of situation and tracking of interventions continues. Next phase responses may include the scaling up of initial responses, adapting them – such as if new tools like vaccines or new vaccines become available – and/ or initiating recovery. As appropriate, for example, if the primary objective is met, a plan may be developed for the post-acute phase and a transition to routine involvement or wind down of involvement.
What next?
Through the framework, Gavi can take decisions to apply a wide and varying range of interventions as appropriate to different scenarios. Any response should consider the potential impact of the threat on routine immunisation and the need for further support. Stockpiling vaccines, advance purchase agreements, exceptional supply chain investments, and dose donations can all be ways of accelerating access to vaccines in a pandemic. Technical assistance, delivery support and health system strengthening are critical enablers for timely, appropriate vaccine use.
In the past, it has been challenging to access funding for interventions during emergencies in a timely manner. For example, it took many months to raise and receive the funds needed to finance COVAX, creating delays that contributed to inequitable global access to vaccines. Gavi is putting in place mechanisms to bring forward and make funding rapidly available to respond to crises. When deployed within a transparent decision-making framework, such mechanisms can enable funds to be released more quickly and facilitate more timely interventions. Robust governance and donor approval procedures are vital in such circumstances. Further discussions will be needed to develop and define these in detail.
Working together to achieve common goals
A key part of a global pandemic response is how global health partners work with each other and implementing countries to harness organisational expertise and make real progress and achieve common goals. The Coalition for Epidemic Preparedness Innovations (CEPI) and other R&D partners are well-placed to monitor, assess, fund and support the vaccine development pipeline for vaccines of diseases with pandemic potential. The Gavi Secretariat, through the Alliance governance model, acts as a convener of a range of functions that enable vaccine access, including market shaping, technical assistance, support for countries, fund- raising, and more. UNICEF's expertise in understanding the vaccine supply landscape, market intelligence, tendering and delivery is invaluable for accelerating vaccine supply. National ministries of health and of finance, public health agencies, and regulators provide critical leadership to enable the delivery of vaccines to populations on the ground.
No one – neither governments nor global/international institutions – was ready for COVID-19. COVAX provided a vital lifeline to many, delivering nearly 2 billion vaccine doses to 146 countries by the end of 2022. There will be future outbreaks of pandemic potential. Governments and agencies must learn from the past so that collaborative approaches to mitigating the impacts of pandemics are faster and more effective in the future.
Gavi is among those working to understand the lessons of COVID-19 as part of its ongoing commitment to maximise its future impact by investing in equitable access to vaccines. Its ground-breaking, life-saving work in routine immunisation, and track record in PPPR and innovative finance, mean Gavi is particularly well-placed to develop and coordinate an effective emergency response decision- making framework for outbreaks of pandemic potential.
Pandemics, epidemics, and outbreaks can be complex, diverse and unpredictable. A decision-making framework is not a panacea. Naturally, there are limits to what such an approach can achieve in a fast-moving health emergency, when data is limited and unreliable, especially when the political stakes are high. However, when built on values-based principles, experience and knowledge sharing, the best-available expert input, appropriate governance, and partners collaborating to use their key competences, a decision-making framework has the potential to improve pandemic response, and therefore to substantially reduce disease burden and save a great many lives.
References
- https://www.cidrap.umn.edu/h1n1-2009-pandemic-
- influenza/study-puts-global-2009-h1n1-infection-rate-11-21
- https://www.medrxiv.org/content/10.1101/2022.10. 11.22280963v1
- https://www.pnas.org/doi/10.1073/pnas.2105482118
- This does not include programmes for which Gavi already has outbreak response measures in place, such as for measles.

